Detection of vector-borne pathogens in dogs with cranial cruciate ligament rupture living in the Mediterranean region
Excerpts from a study by Maria‑Dolores Tabar, Javier Tabar, Carolina Naranjo, Laura Altet and Xavier Roura from 2022
https://doi.org/10.1186/s13071-022-05205-x
translated and shortened by Sven Jan Arndt
Introduction
The detection of vector-borne pathogens in dogs with cranial cruciate ligament rupture living in the Mediterranean region is of great importance for the health and welfare of the animals. Through careful examination and analysis, potential infections can be identified and appropriate measures can be taken to contain the spread of disease.
The role of vectors, such as ticks or fleas, in transmitting pathogens to dogs should not be underestimated. These tiny parasites can transmit various dangerous diseases such as Lyme disease, Ehrlichiosis or Leishmaniasis. Therefore, it is important to develop specific detection methods to identify these pathogens in dogs with cranial cruciate ligament rupture in the Mediterranean region.
Effective diagnosis requires a combination of different techniques and tests. These include, for example, serological tests, molecular examinations such as polymerase chain reaction (PCR) or clinical examinations to detect symptoms and signs of an infection. This comprehensive approach allows an accurate diagnosis to be made and appropriate treatment to be initiated.
Detection of vector-borne pathogens in dogs with cranial cruciate ligament rupture in the Mediterranean region requires close collaboration between veterinarians, laboratories and research institutions. Only through joint efforts can we deepen our understanding of these diseases, develop preventive measures and improve canine health.
Overall, the detection of vector-borne pathogens in dogs with cranial cruciate ligament rupture in the Mediterranean region would be an important step to contain the spread of infections and ensure the welfare of the animals.
background
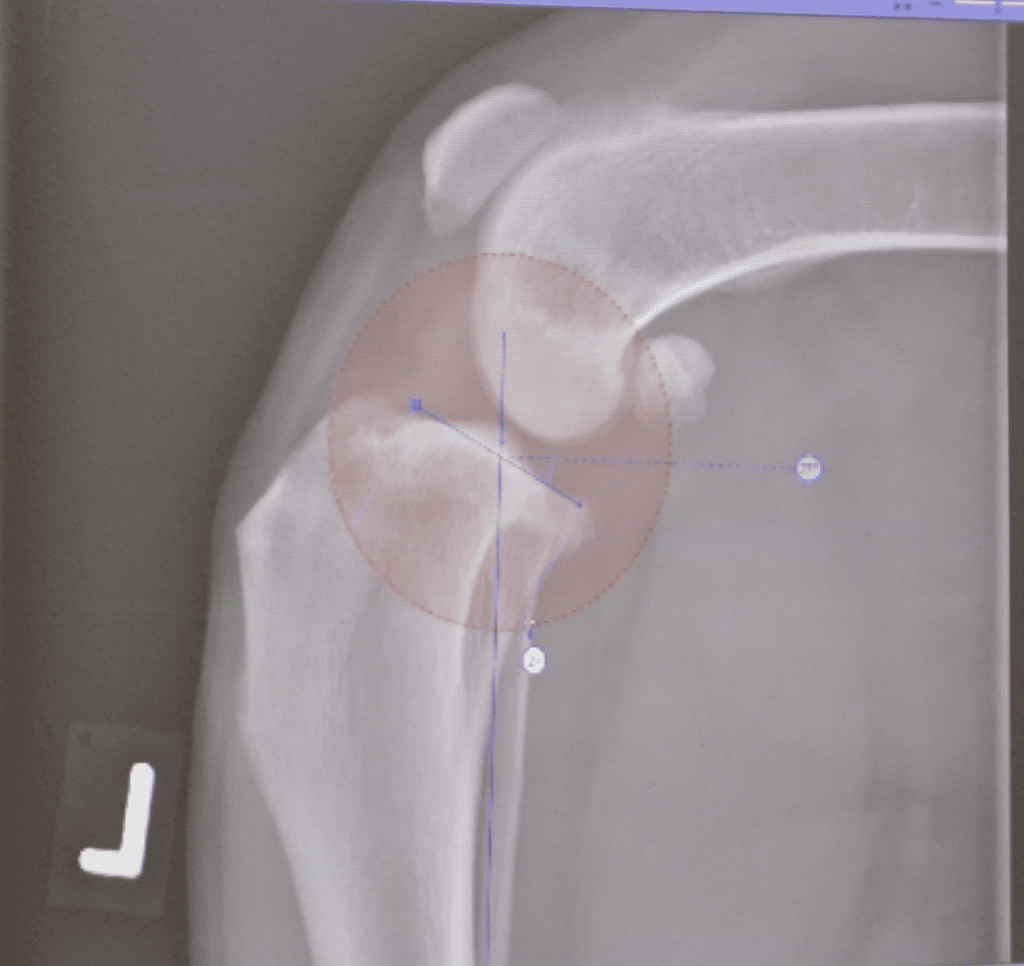
Cranial cruciate ligament rupture ( CCLR ) is a common cause of pelvic limb lameness in dogs, most often due to a degenerative process that results in rupture of the ligament. Several risk factors have been described, such as age, breed, gender, spay status, and weight [1,2]. CCLR is believed to have a multifactorial origin involving genetics, anatomy, and chronic joint inflammation, eventually leading to ligament rupture and osteoarthritis [3, 4].
It has been suggested that immunopathological mechanisms may be involved in the development of degenerative CCL lesions [5], and furthermore, lymphoplasmacytic synovitis is a common finding in dogs with CCLR [6]. Therefore, two hypotheses have been proposed about the role of chronic synovitis in the development of cruciate ligament fiber damage and, consequently, CCLR. The first hypothesis is that synovitis is a near-primary event leading to progressive destruction of the ligamentous fibers [7].
The second reason is that several inherent previous publications reported increased bacterial burden of the synovial membrane in biopsies of inflamed knee joints from dogs with CCLR compared to healthy knee joints, suggesting that environmental bacteria may trigger persistent chronic synovitis [8 , 9]. Other types of pathogens, such as Other pathogens, such as vector-borne pathogens (VBP), can cause acute and chronic joint diseases in dogs, but their role in CCLR has not been thoroughly investigated [10-14].
In a recent study in Brazil, it was reported that 91.3% of 46 dogs with leishmaniasis had joint abnormalities detected on physical examination, x-ray and/or computed tomography, but CCLR was not in the list of those described Joint abnormalities included [14]. Other VBPs such as Ehrlichiacanis, Anaplasma phagocytophilum, Rickettsiarickettsii, Borrelia burgdorferi, Babesia canis, Bartonellavinsonii subsp. berkhoffii and filariae have also been associated with joint diseases such as: B. Polyarthritis, in dogs [4,10, 15-24].
The aim of this study is to detect multiple VBPs in dogs with CCLR, determine whether there is a relationship between the presence of VBP and CCLR, and determine the presence of a specific inflammatory pattern in the synovial membrane of dogs with CCLR and VBP.
Methods
This was a prospective study involving 46 dogs presented for surgical treatment of CCLR and 16 control dogs euthanized due to conditions unrelated to the joints. Samples collected included blood, synovial fluid, and a synovial membrane biopsy.
Pathogen testing included serology for Leishmania infantum (quantitative ELISA), Ehrlichiacanis/ewingii, Borrelia burgdorferi, Anaplasma phagocytophilum/platys and Dirofilaria immitis (4DX IDEXX test) as well as PCR for L. infantum, Ehrlichia/Anaplasma spp, Bartonella spp., piroplasms (Babesia spp. and Theileria spp.) and filariae (D. immitis, Dirofilaria repens, Acanthocheilonema dracunculoides, Acanthocheilonema reconditum and Cercopithifilariaspp.) in EDTA whole blood (EB) and synovial fluid (SF) samples. In addition, SF cytology and histopathological evaluation of the synovial membrane were performed.
Results
The study included 62 dogs, 46 with CCLR and 16 control dogs. Twenty-five female dogs (17 intact and eight neutered) and 21 male dogs (15 intact and six neutered) aged 6 months to 11 years were affected by CCLR. There were 16 different breeds, the most common being mixed-breed dogs (n = 18). In the control group there were eight female dogs (four intact and four neutered) and eight male dogs (six intact and two neutered) aged 4 to 17 years and 10 different breeds (Additional file 1: Table S1).
Reasons for euthanasia included neoplasia (five), chronic renal failure (two), gastric dilatation-volvulus (one), pituitary hyperadrenocorticism (one), disc herniation (two), urethral obstruction (one), heart failure (two), refractory epilepsy (one). and acute liver failure (one).
None of the dogs included in this study had a clinical history, clinical signs, or clinicopathological abnormalities suggestive of VBP infection. The prevalence of VBP in the CCLR group was 19.6% (9/46). Leishmania infantum was detected in six dogs, three of which were seropositive, one was SF-PCR positive, and two were both seropositive and SF-PCR positive. Ehrlichia spp. were detected in three dogs, two of which were seropositive and one was seropositive and blood PCR positive (E. canis).
One of these dogs was infected with L. infantum (SF-PCR positive) and Ehrlichia spp. co-infected (seropositive). Finally, Theileriaequi DNA was detected in the SF sample of a dog (Additional file 2: Table S2). In the control group, the prevalence of VBP in dogs was 18.8% (3/16). All three dogs were positive for L. infantum, one seropositive, one blood PCR positive and one seropositive and both blood and SF PCR positive (Additional file 2: Table S2). No VBPs were detected by light microscopy in a SF smear from any of the dogs included in this study, and the overall prevalence of VBPs was not statistically different between dogs with CCLR and control dogs [odds ratio (OR) = 0.949, 95% confidence interval (CI) 0.22-4.05, P = 0.629].
Unilateral CCLR was found in 29 dogs (five of them with VBP), while CCLR occurred bilaterally in 17 dogs (four of them with VBP), meaning that the presence of bilateral CCLR was not statistically more common in dogs with VBP (OR = 0.677, 95% CI 0.15-2.97, P = 0.439). Histopathological examination of synovial membrane biopsies revealed synovitis with various inflammatory patterns including lymphoplasmacytic (17), neutrophilic (one), granulomatous (one), and mixed lymphoplasmacytic and granulomatous (two) in 45.6% (21/46) of dogs with CCLR ); and in 43.7% (7/16) of control dogs, all of which had lymphoplasmacytic infiltration.
The presence of synovitis was not statistically more common in dogs with CCLR compared to control dogs (χ2 = 0.017, df = 1, P = 0.895) or in dogs with or without VBP (χ2 = 0.141, df = 1, P = 0.708). In addition, no different or specific inflammatory pattern was found in dogs with VBP, regardless of whether they had CCLR or were control dogs (Additional file 2: Table S2). When reviewing the results of VBP-positive dogs with CCLR, two of three dogs with L. infantum PCR positive, but without prior clinical history or diagnosis of Leishmania infection, developed clinical signs suggestive of overt leishmaniasis between 9 and 12 months after CCLR surgery (Additional file 2:Table S2).
discussion
This study failed to demonstrate a role for VBP in CCLR nor the presence of a specific pattern of joint inflammation in VBP-positive dogs, although several vector-borne diseases have been associated with joint damage in dogs [4, 10, 14, 16 -22, 24] and some of them, especially leishmaniasis, are considered endemic in the area where the present study was conducted [28].
Larger case-control studies would likely be required to clarify the role of various vector-borne organisms as a cause or cofactor in the development of CCLR. In canine leishmaniasis, an incidence of orthopedic problems ranging from 44.8% to 91.3% has been reported when both orthopedic examination and imaging (radiology and/or computed tomography) were combined to screen for joint abnormalities [14, 29 ]. Abnormalities noted on orthopedic examination include joint stiffness, lameness, soft tissue swelling, joint pain or crepitus, and functional disability.
Dogs with CCLR may have one or more of these described orthopedic anomalies, but in previous studies there was no specific information about the prevalence of CCLR in dogs suffering from leishmaniasis. Theoretically, the lameness in leishmaniasis could be caused by polyarthritis with additional bone or muscle involvement, usually secondary to inflammation associated with the deposition of immune complexes in the joint due to a type III hypersensitivity reaction [4, 12, 30].
However, primary joint infection can also occur, and the parasites have been identified in macrophages by cytological examination of synovial fluid and by histological examination of synovial membranes [31, 32]. Thus, infected dogs may present with monoarthritis, oligoarthritis or polyarthritis [18], and according to some reports, the knee joint may be affected in almost 80% of cases [14]. In this study, L. infantum was the most common VBP detected in dogs with CCLR, although its prevalence was not significantly different from that of control dogs, suggesting that Leishmania infection does not play a role in the pathogenesis of CCLR.
A possible explanation for the detection in both groups of dogs could be the high prevalence of subclinical infection in a leishmaniasis-endemic area [28, 33].
An association between polyarthritis and Ehrlichiosis has been reported previously; however, there was no clear evidence for this and other possible co-infections were not excluded, so the association was controversial [10, 15-17]. In the present study, Ehrlichia antibodies or DNA were detected in three dogs with CCLR. However, infection could not be confirmed in the only two seropositive dogs, which may simply be due to exposure or previous infection. The third dog, which was seropositive and E. canis PCR positive, had no other clinical symptoms or laboratory abnormalities suggestive of overt or subclinical Ehrlichiosis before or after CCLR surgery.
This could indicate that the dog was either in an acute stage of the disease and recovered on its own, or that it was in a subclinical stage. Both scenarios likely exclude a link between CCLR and Ehrlichia infection.Theileria equi is one of the equine piroplasmas that is enzootic in Spain, with almost half of horses having antibodies or circulating parasitemia [34].
This parasite has occasionally been detected in dogs, but its epidemiological and clinical significance remains unknown [35]. All this and the fact that the dog in this study with T. equi in SF had no other clinicopathological abnormalities throughout the study period may indicate that this pathogen was opportunistic and had no clinical significance for CCLR.
Although Bartonella, A. phagocytophilum, B. burgdorferi, Filariae or other piroplasms such as Babesia have been associated with acute or chronic canine polyarthritis [10, 13, 17, 19-22, 36], no dogs in this study were positive for any of these pathogen. These results may be consistent with the local geographical prevalence of these VBPs found in previous studies in the area examined in this study [16, 27, 34, 37].
However, it should be noted that the limited sensitivity of the techniques used and the limitations associated with the samples taken for the study may also have contributed to the inability to detect these organisms. Lymphoplasmacytic arthritis was the most common histopathological finding in this study, both in dogs with and without CCLR. This is consistent with previous publications in which lymphoplasmacytic synovitis was commonly described in dogs with CCLR [6], but it has also been detected in postmortem samples from dogs without CCLR [7].
On the other hand, reactive immune-mediated arthritis is predominantly neutrophilic due to the deposition of developed immune complexes as a result of VBP infection [4, 11, 12, 18, 29]. This fact reinforces the idea that VBP plays no role in the pathogenesis of CCLR, along with the fact that neither the inflammatory pattern nor the frequency of synovitis was statistically different between dogs with or without CCLR or between dogs with or without VBP in this study .
Although not statistically significant, three dogs with CCLR in this study showed granulomatous synovitis, a type of inflammation also observed in several tissues of leishmaniasis patients [33, 38], but only one of these was positive for leishmaniasis. Although granulomatous inflammation is usually associated with the presence of Leishmania in tissue [12, 13], no amastigotes were detected in this seropositive and LeishmaniaPCR-positive dog with granulomatous synovitis.
The cause of the granulomatous inflammation in the other two dogs remains unclear. Therefore, in the current study, a possible role of these VBPs in the pathogenesis of synovitis and perhaps also CCLR in some of these dogs could not be definitively excluded. This study has some limitations. The small number of dogs included, due to the difficulties in recruiting cases due to the strict inclusion criteria and the fact that this was a prospective study with a control group, means that the statistical results should be treated with caution.
Additionally, only dogs that received surgical treatment for CCLR were included, so dogs that were initially diagnosed with VBP and CCLR and ultimately did not undergo surgery were excluded. Another limitation was the variety of diseases that led to the euthanasia of the control dogs and the fact that joint surfaces were not evaluated, particularly since the control population had a higher average age.
However, the medical history was comprehensively evaluated to exclude previous infections with ÖVPP or diseases that could affect the joints. Additionally, the control dogs were examined during the same time period and in the same area as the CCLR dogs, so the likelihood of detecting VBP was not as influenced. The final limitation concerned the determination of the presence of VBP. In this study, we used serology, microscopy in SF cytology and synovial membrane biopsy, as well as PCR in blood and SF to maximize the probability of VBP detection.
However, the positive serologies were not proof of the causality of the abnormalities found in the joint. Furthermore, it was not possible to perform serology for all pathogens sought, nor could immunohistochemistry and/or PCR be performed on the biopsy to increase the probability of detecting selected VBPs.
Conclusions
This study failed to demonstrate a role for different VBPs in the pathogenesis of CCLR in dogs nor the presence or different pattern of joint inflammation in pathogen-positive dogs. However, to overcome the limitations of this study, further studies may be required to clarify the possible association between VBP and CCLR in dogs.
Sources
1. Brioschi V, Arthurs GI. Cranial cruciate ligament rupture in small dogs (<15kg): a narrative literature review. J Small Anim Pract. 2021;62:1037–50.
2. Gilbert S, Langenbach A, Marcellin-Little DJ, Pease AP, Ru H. Stifle joint osteoarthritis at the time of diagnosis of cranial cruciate ligament injuryis higher in Boxers and in dogs weighing more than 35 kilograms. Vet Radiol Ultrasound. 2019;60:280–8.
3. Comerford EJ, Smith K, Hayashi K. Update on the etiopathogenesis of canine cranial cruciate ligament disease. Vet Comp Orthop Traumatol. 2011;24:91–8.
4. Bennett D. Immune-mediated and infectious arthritis. In: Ettinger SJ, Feldman EC, editors. Textb Vet Intern Med Dis Dog Cat. 7th ed. Missouri: Saunders; 2010. p. 743–9.
5. Doom M, de Bruin T, de Rooster H, van Bree H, Cox E. Immunopathological mechanisms in dogs with rupture of the cranial cruciate ligament. Vet Immunol Immunopathol. 2008;125:143–61.
6. Erne JB, Goring RL, Kennedy FA, Schoenborn WC. Prevalence of lymphoplasmacytic synovitis in dogs with naturally occurring cranial cruciate ligament rupture. J Am Vet Med Assoc. 2009;235:386–90.
7. D.ring AK, Junginger J, Hewicker-Trautwein M. Cruciate ligament degeneration and stifle joint synovitis in 56 dogs with intact cranial cruciate ligaments: correlation of histological findings and numbers and phenotypes of inflammatory cells with age, body weight and breed. Vet Immunol Immunopathol. 2018;196:5–13.
8. Muir P, Oldenhoff WE, Hudson AP, Manley PA, Schaefer SL, Markel MD, et al. Detection of DNA from a range of bacterial species in the knee joints of dogs with inflammatory knee arthritis and associated degenerative anterior cruciate ligament rupture. Microb Pathog. 2007;42:47–55.
9. Schwartz Z, Zitzer NC, Racette MA, Manley PA, Schaefer SL, Markel MD, et al. Are bacterial load and synovitis related in dogs with inflammatory stifle arthritis? Vet Microbiol. 2011;148:308–16.
10. Foley J, Drazenovich N, Leutenegger CM, Chomel BB. Association between polyarthritis and thrombocytopenia and increased prevalence of vectorborne pathogens in Californian dogs. Vet Rec. 2007;160:159–62.
11. Stull JW, Evason M, Carr AP, Waldner C. Canine immune-mediated polyarthritis: clinical and laboratory findings in 83 cases in western Canada (1991–2001). Can Vet J. 2008;49:1195–203.
12. Day MJ. The immunopathology of canine vector-borne diseases. Parasite Vectors. 2011;4:48.
13. Koutinas AF, Koutinas CK. Pathologic mechanisms underlying the clinical findings in canine leishmaniasis due to Leishmania infantum/chagasi. Vet Pathol. 2014;51:527–38.
14. Silva ARS, Oliveira HS, Gomes AAD, Beserra HEO, Silva JP, Santos-Doni TR, et al. Joint involvement in canine visceral leishmaniasis: orthopedic physical examination, radiographic and computed tomographic findings. Vet Parasitol. 2021;299:109569.
15. Bellah JR, Shull RM, Selcer EV. Ehrlichia canis-related polyarthritis in a dog. J Am Vet Med Assoc. 1986;189:922–3.
16. Sainz A, Roura X, Mir. G, Estrada-Pea A, Kohn B, Harrus S, et al. Guidelines for veterinary practitioners on canine Ehrlichiosis and anaplasmosis in Europe. Parasite Vectors. 2015;8:75.
17. Zandvliet MM, Teske E, Piek CJ. Ehrlichia and Babesia infections in dogs in The Netherlands. Tijdschr Diergeneeskd. 2004;129:740–5.
18. Sbrana S, Marchetti V, Mancianti F, Guidi G, Bennett D. Retrospective study of 14 cases of canine arthritis secondary to Leishmania infection. J Small Anim Pract. 2014;55:309–13.
19. Eberts MD, Diniz PPVP, Beall MJ, Stillman BA, Chandrashekar R, Breitschwerdt EB. Typical and atypical manifestations of Anaplasma phagocytophilum infection in dogs. J Am Anim Hosp Assoc. 2011;47:e86-94.
20. Hodges S, Rishniw M. Intraarticular Dirofilaria immitis microfilariae in two dogs. Vet Parasitol. 2008;152:167–70.
21. Gabrielli S, Giannelli A, Brianti E, Dantas-Torres F, Bufalini M, Fraulo M, et al. Chronic polyarthritis associated to Cercopithifilaria bainae infection in a dog. Vet Parasitol. 2014;205:401–4.
22. P.rez C, Maggi RG, Diniz PPVP, Breitschwerdt EB. Molecular and serological diagnosis of Bartonella infection in 61 dogs from the United States. J Vet Intern Med 2011;25:805–10.
23. Rondeau MP, Walton RM, Bissett S, Drobatz KJ, Washabau RJ. Suppurative, nonseptic polyarthropathy in dogs. J Vet Int Med 2005;19:654–62.
24. Mylonakis ME, Soubasis N, Balakrishnan N, Theodorou K, Kasabalis D, Saridomichelakis M, et al. Molecular identification of Bartonella species in dogs with leishmaniosis (Leishmania infantum) with or without cytological evidence of arthritis. Vet Microbiol. 2014;174:272–5.
25. Francino O, Altet L, Sanchez-Robert E, Rodriguez A, Solano-Gallego L, Alberola J, et al. Advantages of real-time PCR assay for diagnosis and monitoring of canine leishmaniasis. Vet Parasitol. 2006;137:214–21.
26. Movilla R, Altet L, Serrano L, Tabar MD, Roura X. Molecular detection of vector-borne pathogens in blood and splenic samples from dogs with splenic disease. Parasite Vectors. 2017;10:131.
27. Martínez V, Quilez J, Sanchez A, Roura X, Francino O, Altet L. Canine leishmaniasis: the key points for qPCR result interpretation. Parasite Vectors. 2011;4:57.
28. Me. G, Montoya A, Roura X, G.lvez R, Sainz A. Seropositivity rates for agents of canine vector-borne diseases in Spain: a multicenter study. Parasite Vectors. 2013;6:117.
29. Agut A, Corzo N, Murciano J, Laredo FG, Soler M. Clinical and radiographic study of bone and joint lesions in 26 dogs with leishmaniasis. Vet Rec. 2003;153:648–52.
30. Sappendel RJ, Ferrer L. Leishmaniosisa. In: Greene CE, editor. Infect Dis Dog Cat. Philadelphia: Saunders; 1990. p. 450–7.
31. Lennox WJ, Smari ME, Littke PB. Canine leishmaniasis in Canada. Can Vet J 1972;13:188–90.
32. Turrel JM, Pool R. Bone lesions in four dogs with visceral leishmaniasis. Vet Radiol. 1982;23:243–9.
33. Solano D, Mir. G, Koutinas A, Cardoso L, Pennisi MG, Ferrer L, et al. The LeishVet group. LeishVet guidelines for the practical management of canine leishmaniasis. Parasite Vectors. 2011;4:86.
34. Camino E, Buendia A, Dorrego A, Pozo P, de Juan L, Dominguez L, et al. Sero-molecular survey and risk factors of equine piroplasmosis in horses in Spain. Equine Vet J. 2021;53:771–9.
35. Solano-Gallego L, Sainz A, Roura X, Estrada-Pe.a A, Mir. G. A review of canine babesiosis: the European perspective. Parasite Vectors. 2016;9:336.
36. Shaw SE, Day MJ, Lerga A, Birtles RJ, Kenny MJ. Anaplasma (Ehrlichia) phagocytophila: a cause of meningoencephalitis/polyarthritis in dogs? J Vet Intern Med. 2002;16:636.
37. Tabar MD, Francino O, Altet L, Sanchez A, Ferrer L, Roura X. PCR survey of vectorborne pathogens in dogs living in and around Barcelona, an area endemic for leishmaniasis. Vet Rec. 2009;164:112–6.
38. Pe.a MT, Naranjo C, Klauss G, Fondevila D, Leiva M, Roura X, et al. Histopathological features of ocular leishmaniasis in the dog. J Comp Pathol. 2008;138:32–9.
