Canine Epilepsy: Comprehensive Guide to Diagnosis and Treatment
- Canine Epilepsy: Comprehensive Guide to Diagnosis and Treatment
- Introduction to epilepsy in dogs
- Epilepsy in dogs: definition and frequency
- Epilepsy types and symptoms
- Diagnosis of epilepsy in dogs
- Therapy of epilepsy in dogs
- No need for therapy for epilepsy in dogs
- Treatment-resistant epilepsy in certain dog breeds
- Frequently asked questions about epilepsy in dogs
- When is it better to let the dog with epilepsy go?
- Summary
Introduction to epilepsy in dogs
Epilepsy is a disease that occurs not only in humans but also in our pets, especially dogs. It is a neurological disorder characterized by repeated seizures caused by a temporary malfunction of brain cells. It is a complex disease that requires accurate diagnosis and tailored treatment to ensure that affected dogs live a good and healthy life.
Epilepsy in dogs: definition and frequency
Canine epilepsy, also known as epilepsy, is one of the most common neurological diseases, affecting approximately 2% of all dogs. This disease can occur at any age, from puppies to seniors.
Canine epilepsy is a brain dysfunction that disrupts the balance between electrical charge and discharge in nerve cells. This results in uncontrolled electrical impulses that cause the brain to respond to this excess activity with an epileptic seizure. These attacks can vary in severity and in most cases end on their own.
Epilepsy types and symptoms
Epileptic seizures can be divided into two main groups depending on their origin: partial or focal epilepsy and generalized epilepsy.
Partial or focal epilepsy in dogs
Canine partial or focal epilepsy is a form of canine epilepsy characterized by seizures that begin in a specific area of the brain and affect a specific area of the body. Unlike generalized epilepsy in dogs, in which seizures affect both hemispheres of the brain, seizures in focal epilepsy are limited to a specific part of the brain.
Partial seizures can have different symptoms depending on the area of the brain affected. These may include motor symptoms (such as twitching movements of a particular body part), sensory symptoms (such as changes in visual, hearing or smell sensations), autonomic symptoms (such as a racing heart or sweating), or psychological symptoms (such as anxiety or euphoria). In some cases, these seizures can also lead to complex behavioral changes, including so-called automatic behaviors in which the sufferer makes repetitive and uncontrolled movements.
There are two main types of partial seizures: simple and complex. In simple focal seizures, consciousness is retained, while in complex focal seizures, consciousness is impaired or lost. In some cases, focal seizures can become secondarily generalized, meaning that they spread from a specific area of the brain to the entire brain and become a generalized seizure.
The exact cause of focal epilepsy in dogs is often unknown, but there are many factors that can contribute to the development of this condition, including genetic factors, brain injury, stroke, tumors, and central nervous system infections.
Diagnosing canine focal epilepsy can be challenging because symptoms are highly variable and can be difficult to distinguish from other neurological disorders. The diagnosis is usually based on a careful history, neurological examinations and imaging techniques such as magnetic resonance imaging (MRI) or computed tomography (CT).
Treatment of focal epilepsy in dogs is primarily aimed at reducing the frequency and severity of seizures and improving the patient's quality of life. This can be achieved through medication, surgery, dietary adjustments, or behavior changes.
It is important to emphasize that the prognosis for individuals with focal epilepsy can vary greatly depending on the cause and severity of the condition. However, with proper treatment and support, many people with this condition can lead full and productive lives.
Generalized epilepsy
Generalized canine epilepsy is a form of epilepsy that affects both hemispheres of the brain and affects the animal's entire body. It is particularly common in dogs, accounting for around 80% of cases.
Generalized seizures are divided into various subcategories, with the tonic seizure (from tone = tension) being the predominant form in dogs. This seizure can be divided into three phases:
- Prodromal phase: This phase, which can occur hours or even days before the actual seizure, is characterized by behavioral changes that may indicate an impending seizure. The dog may be restless, anxious or clingy.
- Ictal phase: The actual seizure occurs in this phase. During a tonic seizure, the dog freezes, falls over, and may lose consciousness. Stiff movements of the limbs may occur, often accompanied by excessive salivation, urine and feces. This phase usually lasts between a few seconds to a few minutes.
- Postictal phase: This is the phase after the seizure. The dog may be confused and disoriented and may have temporary visual impairment. Recovery can last from a few minutes to several hours.
Epilepsy in dogs - an example - not for sensitive souls!
It is important to note that the animal's owner should remain calm during a seizure and give the dog as much space as possible to avoid injury. Reaching into the dog's mouth during a seizure is not recommended as it can be dangerous for both the dog and the owner.
The diagnosis of generalized epilepsy in dogs is usually made by excluding other causes of the seizures, such as metabolic disorders, infections or tumors. The exact cause of generalized epilepsy is often unknown, but it is thought that both genetic and environmental factors may play a role.
Treatment of generalized epilepsy in dogs consists primarily of reducing the frequency and severity of seizures. This includes medications such as anticonvulsants and benzodiazepines, an adjusted diet and stress management. It is important to regularly monitor and adjust treatment to achieve optimal results and minimize side effects.
In summary, generalized epilepsy in dogs is a serious but treatable condition. With an accurate diagnosis and appropriate treatment, affected dogs can lead normal and happy lives.
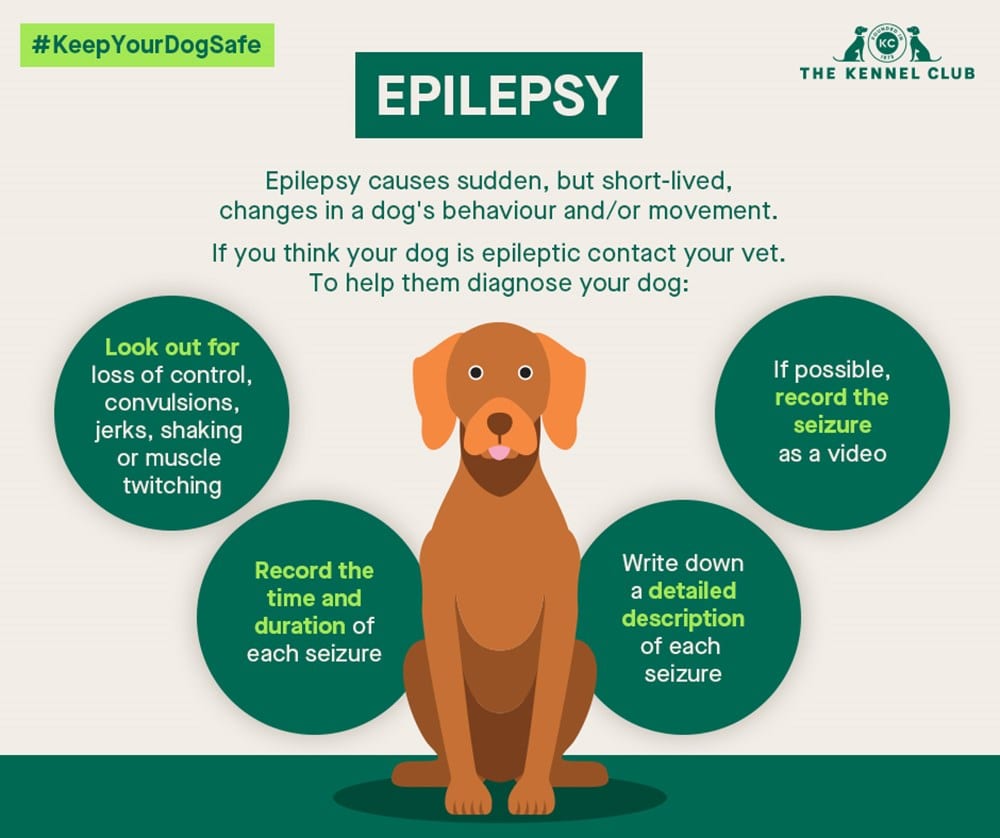
Diagnosis of epilepsy in dogs
Diagnosing epilepsy in dogs can be challenging because symptoms vary and must be differentiated from other neurological and non-neurological diseases. There are no specific tests that allow a definitive diagnosis of epilepsy in dogs, so diagnosis relies on a careful history, clinical examinations and exclusion procedures.
During the anamnesis, the veterinarian ask the owner about the specific symptoms, their frequency and duration, as well as possible triggering factors. It is important that the owner describes as accurately as possible the type of seizure, the dog's behavior before, during and after the seizure, and any change in the dog's general condition or behavior.
The clinical examination includes a general health check and a neurological examination. The veterinarian will examine the dog for signs of an underlying medical condition that could be causing seizures, including infections, poisoning, metabolic disorders, or tumors.
In addition, various diagnostic tests may be performed to rule out other causes of seizures and identify possible associated symptoms. These include blood tests, urinalysis, x-rays, ultrasound scans and more specialized tests such as electroencephalography (EEG) or imaging tests such as magnetic resonance imaging (MRI) or computed tomography (CT). In some cases, a CSF examination (examination of the cerebrospinal fluid) may be necessary.
In dogs in which no other cause for the seizures is found, a diagnosis of idiopathic or primary epilepsy may be made. This is a genetic form of epilepsy in dogs that is more common in certain breeds and usually begins between the ages of one and five.
It is important to note that diagnosing canine epilepsy requires a detailed and often time-consuming examination. A single epileptic event does not necessarily mean that the dog has epilepsy. Rather, the diagnosis is usually made when the dog has had multiple unprovoked seizures at least 24 hours apart.
The prognosis for dogs with epilepsy can vary and depends on factors such as the severity and frequency of seizures, the dog's age at onset of the disease, the presence of other health problems, and response to treatment.
Therapy of epilepsy in dogs
Therapy for canine epilepsy aims to reduce the frequency and severity of seizures and improve the dog's quality of life while minimizing side effects. Specific therapy may vary depending on the dog's individual circumstances, including the type of epilepsy in the dog, the frequency and severity of seizures, the dog's age and general health, and the presence of other diseases.
- Antiepileptic drugs (AEDs): These are the mainstays of treatment and include medications such as phenobarbital, primidone, potassium bromide, levetiracetam and imepitoin. Selecting the most appropriate medication depends on several factors, including the type and severity of seizures, the dog's breed, age, and general health. It is important to note that administration of these medications requires regular monitoring of blood counts and dosage adjustments to ensure optimal effectiveness and minimize side effects.
- Management and lifestyle changes: In some cases, adjustments to the dog's environment and lifestyle can help prevent seizures or reduce their severity. This includes avoiding known triggers, maintaining a regular routine, eating a balanced diet and getting enough exercise.
- Diet therapy: There is some evidence that certain diets, particularly the ketogenic diet, may help reduce seizures in some dogs. However, further research is needed in this area and such a diet should only be implemented under the supervision of a veterinarian or animal nutritionist.
- Surgery and neuromodulative therapy: Surgical intervention may be considered in dogs with focal epilepsy that are unresponsive to medication and have clear structural brain changes. Alternatively, neuromodulatory therapies such as vagus nerve stimulation (VNS) or deep brain stimulation (DBS) may be useful in some cases, although this is rare.
It is important to emphasize that the treatment of epilepsy in dogs requires a long-term commitment and that therapy is usually not aimed at completely eliminating seizures but at reducing their frequency and severity. It is also important to understand that although therapy can usually provide significant improvement, it is not always successful and in some cases, severe and life-threatening seizures can occur despite optimal therapy.
Antiepileptic drugs (AEDs) in the treatment of epilepsy in dogs
Antiepileptic drugs (AEDs) are the cornerstone of the treatment of epilepsy in dogs. Their main task is to reduce the frequency and severity of seizures without causing unwanted side effects. Below are some of the most commonly used AEDs and their features:
- Phenobarbital: This drug has long been the most commonly used AED in the treatment of epilepsy in dogs. It works by dampening the activity of nerve cells in the brain, thereby inhibiting the development and spread of seizures. While phenobarbital is generally well tolerated, side effects such as increased thirst and hunger, weight gain, behavioral changes, and liver damage can occur. Regular monitoring of blood values and adjustment of the dosage are therefore necessary.
- Primidone: Primidone is another traditional AED used in dogs. It is metabolized in the body to phenobarbital and phenylethylmalonamide, both of which have anticonvulsant effects. The side effects are similar to phenobarbital.
- Potassium bromide: Potassium bromide is often used as adjunctive therapy in dogs that do not respond adequately to phenobarbital alone. It may also be used as first-line therapy in dogs for which phenobarbital is contraindicated. The most common side effects are increased thirst and urination, gastrointestinal complaints and behavioral changes.
- Levetiracetam: Levetiracetam is a newer AED that is becoming increasingly popular in dogs. It has a different efficacy profile than traditional AEDs and appears to be well tolerated, with fewer severe side effects. However, it must be administered more frequently (usually three times daily), which may make compliance difficult.
- Imepitoin: Imepitoin is a relatively new medication designed specifically for the treatment of idiopathic epilepsy in dogs. It works by reducing the release of glutamate in the brain, a substance involved in causing seizures. Imepitoin appears to be well tolerated and has a low risk of serious side effects.
When selecting an AED, several factors must be considered, including the type and severity of seizures, the breed and age of the dog, general health, and the presence of comorbidities. Close collaboration between the pet owner and the veterinarian is crucial to create the best possible treatment protocol and maximize the dog's quality of life.
Management and lifestyle changes for canine epilepsy
Management of canine epilepsy involves not only drug therapy, but also a range of lifestyle changes and supportive measures that can help reduce seizures and improve the dog's quality of life.
1. Minimize stress: Stress can be a trigger for epileptic seizures in dogs. Therefore, it is important to avoid stressful situations as much as possible. This may include maintaining a regular routine, gentle handling, avoiding loud noises and excessive excitement, and providing the dog with a quiet and safe place to retreat.
2. Diet and nutrition: Some dogs may benefit from a special diet aimed at reducing seizure frequency. This may include following a high-fat, low-carbohydrate diet (similar to the ketogenic diet used in people with epilepsy), supplementing with certain nutrients such as taurine and omega-3 fatty acids, or avoiding foods known to be seizure triggers , include. However, such a diet should only be introduced under the guidance of an experienced veterinarian.
3. Regular exercise: Regular physical activity can contribute to the dog's overall health and well-being and can help reduce seizures. However, exercise should be moderate and should not result in overheating or excessive fatigue, as this can lead to seizures.
4. Monitoring and documentation: Regular monitoring and documentation of seizures can help recognize patterns and identify possible triggers. This may include keeping a seizure diary, recording the date, time, duration and characteristics of each seizure, as well as possible triggers and changes in the dog's environment or behavior before the seizure.
5. Regular veterinary checks: Regular veterinary monitoring is crucial for the management of epilepsy in dogs. This allows for early detection and treatment of medication side effects and other health problems that may worsen seizures. In addition, regular blood tests can help monitor the effectiveness of the medication and adjust the dosage if necessary.
It is important to emphasize that every dog is individual and what works for one dog may not work for another. Working closely with an experienced veterinarian is therefore crucial to develop the best possible management and treatment protocol for each individual dog.
Diet therapy for epilepsy in dogs
Diet may play an important role in controlling canine epilepsy, although more research is needed to understand the exact mechanisms and optimal diet composition. The idea of diet therapy is based on the concept that certain nutrients and diet compositions can affect the brain and reduce the frequency and severity of seizures.
1. Ketogenic Diet: Similar to humans using a ketogenic diet to treat difficult-to-control epilepsy, such a diet can also be helpful in dogs. The ketogenic diet is a very high-fat, low-carb diet that causes the body to use ketones for energy instead of relying on glucose. This shift in metabolism is thought to have a stabilizing effect on neurons in the brain, reducing seizure frequency. However, it should be noted that such a diet must be strictly followed and introduced under veterinary supervision, otherwise it may have potentially negative effects on the dog's health.
2. Additional Nutrients: Some studies have shown that adding certain nutrients to a dog's diet can potentially be helpful. For example, it has been suggested that taurine, an amino acid found in high concentrations in the brain, may have neuroprotective properties and may help prevent seizures. Likewise, omega-3 fatty acids, known for their anti-inflammatory properties, may be helpful in controlling epilepsy.
3. Avoiding triggers: For some dogs, avoiding certain foods or additives that can serve as triggers for seizures may be helpful. Such triggers can vary from person to person and are often difficult to identify, but common examples could include certain proteins, artificial colors or preservatives.
Dietary therapy is a promising approach to treating epilepsy in dogs, but it should never be considered a replacement for drug therapy unless specifically recommended by a veterinarian. A balanced, nutrient-dense diet is always important for a dog's overall health and well-being and can help support the overall management of dogs with epilepsy.
Surgery and neuromodulative therapy in dogs with epilepsy
Surgery and neuromodulatory therapy represent potential treatment strategies for dogs with epilepsy, particularly those that do not respond to conventional drug therapies. However, these therapeutic options are complex and associated with potential risks and side effects, so a thorough understanding of these therapeutic methods is essential.
1. Surgery: Surgical removal of the seizure focus may be an option for treating epilepsy in dogs in certain cases. This assumes that the seizure focus is limited to a well-defined and accessible area of the brain that can be removed without significantly affecting normal brain function. Surgical methods used to treat epilepsy include lobectomy, in which part of a lobe of the brain is removed, and functional hemispherotomy, in which one hemisphere of the brain is deactivated. These procedures are technically demanding and require specialized expertise in veterinary neurosurgery.
2. Neuromodulative therapy: Neuromodulation involves a series of techniques that influence electrical activity in the brain to reduce seizure frequency. One form of neuromodulative therapy is vagus nerve stimulation (VNS), which involves implanting a device that regularly sends electrical signals to the vagus nerve. This stimulation is thought to reduce seizure activity by affecting signaling in the brain. VNS is widely used in people with difficult-to-treat epilepsy, and there is evidence that it may also be effective in dogs. Other forms of neuromodulatory therapy, such as deep brain stimulation or responsive neurostimulation, are currently being researched in dogs.
Both approaches, surgery and neuromodulative therapy, require careful weighing of the potential benefits against the risks and side effects. Additionally, they are not suitable for all dogs and should only be considered under the guidance of a specialist veterinary neurologist. In any case, the main goal should be to maximize the dog's quality of life and minimize the stress on the dog and its owner.
No need for therapy for epilepsy in dogs
There are situations in which therapy for epilepsy in dogs is not absolutely necessary. The decision to initiate therapy should be based on a thorough assessment of the individual animal and specific circumstances. The following criteria may be considered to determine whether therapy is necessary or not:
1. Frequency and severity of seizures: Not all dogs with epileptic seizures require long-term drug therapy. If the attacks occur infrequently (for example, less than once a month) and are mild, it may be less distressing for the dog to avoid drug therapy.
2. Cause of epilepsy: Sometimes the underlying cause of epilepsy can be treated, eliminating the need for long-term antiepileptic therapy. For example, in epilepsy caused by a brain mass such as a tumor, surgical removal of the mass can stop the seizures.
3. Health status and age of the dog: For older dogs or dogs with other serious health problems, the decision against antiepileptic therapy may be made if the potential side effects of the medication could significantly affect the dog's well-being.
4. Quality of life of the dog and the owner: The decision for or against therapy should always be based on a consideration of the potential benefits and risks, including the impact on the quality of life of both the dog and the owner. For dogs with mild epilepsy that does not affect their daily activities, foregoing therapy may be warranted.
Overall, the decision to begin therapy for a dog with epilepsy is complex and requires careful consideration. to make this decision in consultation with a veterinarian
Treatment-resistant epilepsy in certain dog breeds
Canine refractory epilepsy, also known as refractory epilepsy, is a condition in which a dog does not respond to commonly used antiepileptic drugs. This can be a significant problem for affected dogs and their owners as it can significantly impact the dog's quality of life and make treatment difficult. Some dog breeds appear to be more susceptible to refractory epilepsy, although the exact reasons for this are not yet fully understood.
1. Belgian Shepherd: Studies have shown that Belgian Shepherds may have an increased prevalence of refractory epilepsy. This is thought to be due to a genetic predisposition, although the exact genetic factors affecting this breed have not yet been identified.
2. Border Collie: Border Collies may also have a higher likelihood of developing refractory epilepsy. This could be due to certain breeding lines within the breed being more prone to developing refractory epilepsy.
3. Australian Shepherd: A higher prevalence of refractory epilepsy has also been found in this breed.
4. Labrador Retriever: Labrador Retrievers can also develop treatment-refractory epilepsy.
It is important to note that refractory epilepsy in dogs is not limited to these breeds and can occur in any breed. In addition, the prevalence of refractory epilepsy within a breed varies depending on various factors, including the specific breeding line and the individual genetic characteristics of the dog. Comprehensive genetic testing can help better understand the risk of refractory epilepsy in a particular dog.
It is also important to note that "refractory" does not mean that a dog's epilepsy is untreatable. Instead, it means that traditional treatment methods may not be as effective and that alternative or additional treatment approaches may be necessary.
Frequently asked questions about epilepsy in dogs
What are the first signs of epilepsy in dogs??
The first signs of epilepsy in dogs can be subtle and are often characterized by seizures. These include behavioral changes such as confusion, restlessness or a decrease in responsiveness. Physical symptoms may include tremors, excessive salivation, uncontrolled muscle movements, and loss of consciousness.
How is epilepsy diagnosed in dogs?
The diagnosis of epilepsy in dogs is based primarily on a combination of history, symptoms, and the results of a neurological examination. In some cases, it may be helpful to have additional tests such as blood tests, urinalysis, X-rays, or magnetic resonance imaging (MRI) to rule out other underlying diseases.
How is epilepsy in dogs treated?
Treatment of epilepsy in dogs usually involves administering antiepileptic drugs to control seizures. Other possible treatment options may include lifestyle and dietary changes, physical therapy, and in some severe cases, surgery.
Can my dog with epilepsy live a normal life?
Yes, many dogs with epilepsy are able to live normal and fulfilling lives despite their diagnosis. It is important that the dog is examined regularly by the veterinarian and that treatment plans are strictly followed. With proper care and support, dogs with epilepsy can often keep their seizures well controlled and continue to live happy, healthy lives.
When is it better to let the dog with epilepsy go?
The decision to euthanize a dog with epilepsy is an extremely difficult and personal decision that should be made in close collaboration with the veterinarian. It depends on a number of factors, including the severity and frequency of seizures, the dog's general health, the dog's quality of life, and the dog owner's ability to meet the dog's medical needs.
A dog may need to consider being euthanized if:
- The seizures remain uncontrolled despite appropriate drug treatment and the dog suffers from severe and frequent seizures that significantly affect his quality of life.
- The dog suffers from a serious concomitant disease or complications related to epilepsy that significantly affects his quality of life and cannot be effectively treated.
- The dog exhibits severely impaired behavior or general health that significantly affects its quality of life and cannot be effectively treated.
However, it is important to emphasize that this decision should always be made based on the individual case and circumstances of the dog and its owner. The goal should always be to maximize the dog's well-being and minimize his suffering.
Summary
Canine epilepsy is a neurological disorder characterized by recurrent seizures. Generalized and partial (or focal) epilepsy can occur in dogs. Generalized epilepsy affects the entire brain, while partial epilepsy in dogs is limited to specific areas.
The diagnosis of epilepsy in dogs is usually made through a detailed history, a clinical examination and special diagnostic tests such as EEG and MRI. It is important to rule out other causes of seizures, such as metabolic disorders or tumors.
Treatment of canine epilepsy can be complex and often requires a multimodal approach. Antiepileptic drugs (AEDs) are the basis of treatment. Common AEDs include phenobarbital and imepitoin, but there are other options such as levetiracetam, zonisamide, and gabapentin. The choice of medication depends on many factors, including the type of epilepsy, the dog's individual response, and the side effects of the medication.
Management and lifestyle changes are equally important. Stress reduction, regular exercise, and a healthy sleep-wake cycle can help reduce the frequency and severity of attacks. A special diet may also be beneficial, particularly a ketogenic diet, which encourages the body to use fats instead of glucose for energy.
In some cases, surgical or neuromodulatory therapy may be considered, especially if the medications are ineffective or have serious side effects. This may include resection of brain tissue that triggers the seizures or implantation of a device to electrically stimulate the brain.
Therapy may not be necessary if seizures are infrequent and do not affect the dog's quality of life. Some dog breeds may be resistant to treatment, including Border Collies, Australian Shepherds, Belgian Shepherds, Beagles and Great Danes.
Finally, it is important that dog owners are well informed about epilepsy in dogs and what they should do during and after a seizure. In extreme cases, when the seizures are uncontrollable and the dog's quality of life is severely affected, the decision to euthanasia may be considered, although this is an extremely difficult and personal decision.
State of current research on epilepsy in dogs
Research into canine epilepsy has made significant progress in recent years, although many questions still remain unanswered. Below are some key developments in research:
- Genetics: The discovery of genetic markers for certain forms of epilepsy has increased our understanding of the disease and enabled the development of new therapies. Various studies have identified specific gene mutations associated with epilepsy in certain dog breeds. A better understanding of the genetic basis of epilepsy could help identify risk factors and develop preventative strategies.
- Pharmacogenomics: This field studies how an individual's genetic makeup influences their response to drugs. There is hope that personalized medicine tailored to each dog's genetic constitution could lead to more effective and safer treatments.
- Neuromodulation: Various neuromodulatory techniques, such as deep brain stimulation and vagus nerve stimulation, are being intensively researched. These techniques could offer a promising alternative or complement to medications, especially in treatment-resistant cases.
- Diet therapy: There is increasing evidence that certain diets, particularly the ketogenic diet, may help reduce seizures in some dogs. However, further research is needed to understand the exact mechanisms and which dogs might benefit most from such diets.
It is important to emphasize that although research in this area is progressing rapidly, the findings have yet to be translated into clinical practice. This requires further clinical trials and long-term observations to confirm the safety and effectiveness of the new therapies.
Relevant literature on epilepsy in dogs
Here are some relevant and current specialist literature sources on the subject of epilepsy in dogs:
- "Canine and Feline Epilepsy: Diagnosis and Management" by Luisa De Risio and Simon Platt. This book provides a comprehensive overview of the diagnosis and treatment of epilepsy in dogs and cats and includes current research.
- "Canine Epilepsy: An Owner's Guide to Living With and Without Seizures" by Caroline Levin. This book is aimed at dog owners and provides practical advice on caring for a dog with epilepsy.
- "The Genetic Basis of Canine Epilepsy" by Gary Johnson et al., published in "The Veterinary Journal". This article provides an overview of current research into the genetic causes of epilepsy in dogs.
- “Antiepileptic Drug Therapy in Dogs” by Stephanie McGrath et al., published in “The Veterinary Clinics of North America: Small Animal Practice.” This article provides a detailed overview of the various antiepileptic drugs currently available for the treatment of dogs.
- "Ketogenic Diet in Dogs with Idiopathic Epilepsy" by D. Packer et al., published in "The British Veterinary Journal". This article examines the effects of the ketogenic diet on seizure control in dogs with idiopathic epilepsy.
Please note that these publications on canine epilepsy are in English and there is no German translation. They are also published in journals and books that may not be easily accessible. It is advisable to contact a university library or a veterinary library to access these resources.
