Comprehensive guide to anaplasmosis in animals
introduction
Anaplasmoses are parasitic infectious diseases caused by Anaplasma species and transmitted by ticks. The affected host animals are primarily dogs, but people, sheep, goats, cats, cattle and horses can also be affected. The disease progresses in acute and chronic phases.
Pathogens and transmission
Anaplasmoses are mainly caused by two species of Anaplasma:
- Anaplasma phagocytophilum: Affects granulocytes (white blood cells).
- Anaplasma platys: Affects thrombocytes (blood platelets).
Anaplasma phagocytophilum and Anaplasma platys belong to the order Rickettsia and are therefore bacteria. Anaplasma phagocytophilum is zoonotic and causes human granulocytic Ehrlichiosis in humans.
vectors and hosts
Anaplasma phagocytophilum is mainly transmitted by shield ticks of the genus Ixodes, in Europe particularly by the wood tick (Ixodes ricinus). Anaplasma platys, on the other hand, is transmitted by the brown dog tick (Rhipicephalus sanguineus).
Transmission of anaplasma usually occurs 24 hours after the tick begins to suck. The incubation period is 5 to 20 days.
distribution
Anaplasma phagocytophilum is distributed between 40th and 65th parallel, including Germany, Sweden, Norway, England, Holland, Poland, Hungary, Austria, Switzerland, Czech Republic, Slovenia, Croatia, Bulgaria, France, northern Spain, northern Italy and northern Romania.
Anaplasma platys occurs in North Africa, southern and central Portugal, southern Spain, Italy, Greece, Gibraltar, Bulgaria, Croatia and southern Romania.
diagnosis
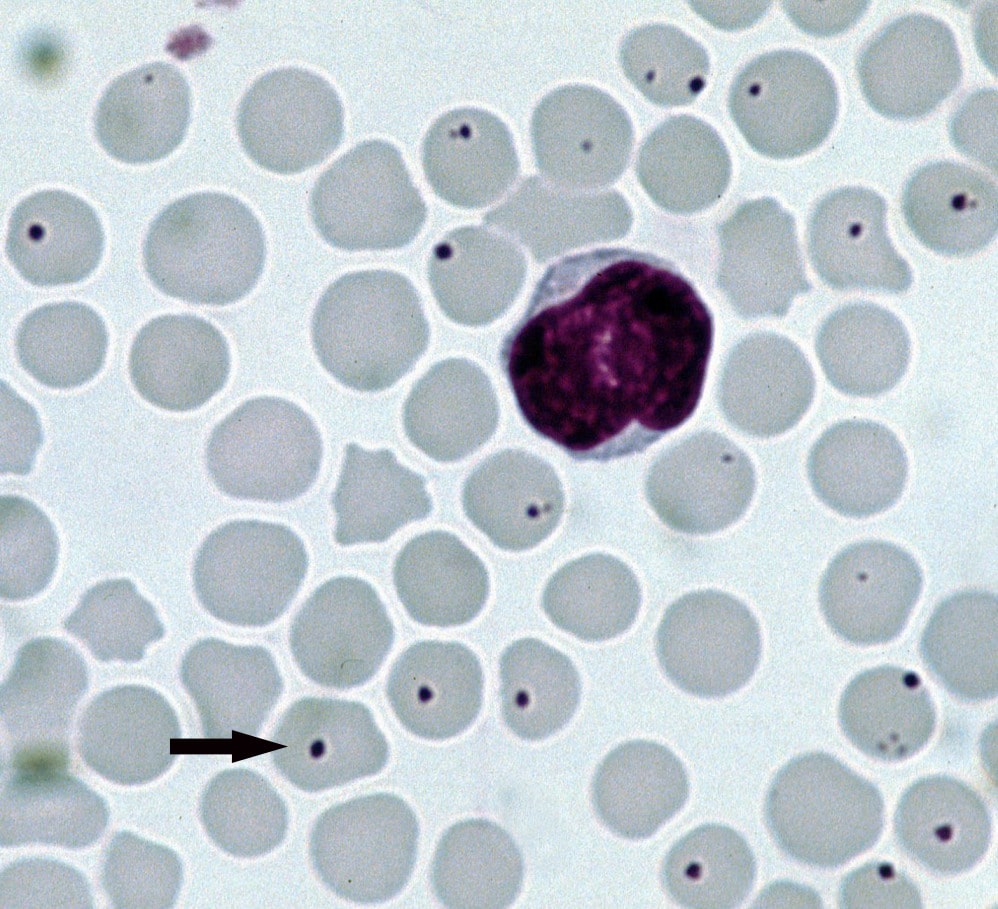
Anaplasmosis is diagnosed by a veterinarian in the acute phase through direct detection of the pathogen using a Giemsa-stained blood smear and/or PCR from blood. In the chronic phase, the pathogen can be detected indirectly by detecting antibodies (titer) using IFAT or ELISA. However, a negative PCR result does not rule out illness.
Diagnosis of anaplasmosis in dogs
Because the symptoms of anaplasmosis can be similar to those of other diseases, such as babesiosis or Lyme disease, it is important to make an accurate diagnosis. Veterinarians use blood tests to detect the presence of Anaplasma bacteria or antibodies against these bacteria. A combination of clinical symptoms, pathogen detection and response to therapy is crucial for the diagnosis.
Symptoms
Acute phase (1-3 weeks)
- Fever
- Apathy, lethargy
- Gastrointestinal disorders
- Splenomegaly (enlarged spleen)
- Lymphadenopathy (swollen lymph nodes)
- Thrombocytopenia (reduced platelet count)
- Nosebleeds, bleeding gums
- Petechiae (small hemorrhages in the skin)
- Lameness
- Polyarthritis (inflammation of multiple joints)
Chronic phase
- Pancytopenia (reduced number of all blood cells)
- Uveitis (inflammation of the eyes)
- Lameness
- Polyarthritis
- Neurological disorders
The symptoms of anaplasmosis are often similar to those of Ehrlichiosis.
Anaplasmosis in Dogs: Common Symptoms and Signs
Symptoms of anaplasmosis infection in dogs can vary, but some of the most common signs include:
- languor
- Fever
- Mucous membrane bleeding (e.g. on the gums)
- Nosebleeds
- Reluctance to move
- Lameness
In rare cases, neurological symptoms such as coordination problems or seizures may also occur.
Laboratory tests
In the acute phase of anaplasmosis, blood tests usually show thrombocytopenia (reduced platelet count), a decrease in lymphocytes and an increase in monocytes, total protein (TP), γ-globulins and C-reactive protein (CRP). As the disease progresses, a reduction in erythrocytes and hematocrit as well as an increase in liver enzymes (ALT, AST) can also occur.
Treatment
In the event of acute symptoms and corresponding changes in the blood count, the veterinarian with an antibiotic. However, pathogen elimination is often not possible for Anaplasma platys, whereas pathogen elimination is possible for Anaplasma phagocytophilum.
In the chronic phase, regular monitoring with blood counts, clinical chemistry and protein electrophoresis is recommended. It should be noted that doxycycline hyclate can cause severe mucous membrane irritation. The tablets should therefore never be administered on an empty stomach, but should be given together with food (e.g. in a meat bag or a chicken heart).
Systemic cortisone therapy is generally contraindicated in vector-based diseases and may only be carried out after a strict risk-benefit assessment. Any co-infections must always be treated at the same time.
prevention
Permethrin-containing and flumethrin-containing spot-ons and/or collars can be used to prevent anaplasmosis. Behavioral prophylaxis consists of avoiding tick-tick areas. In this case, you should seek advice from a veterinarian before traveling.
In addition to tick anti-tick medications, natural supplements such as cistus tablets can be used to further reduce the risk of tick infestation. It is also important to check your dog for ticks regularly, especially after nature walks. If you spot a tick, remove it as quickly as possible with tick tweezers to minimize contact time with the bloodsucker.
Environment and risk factors for anaplasmosis
Because ticks are more common in certain environments, such as tall grasses, bushes, and forests, you should avoid such areas or thoroughly search your dog after being in such environments. The risk of anaplasmosis is highest during the typical tick season from spring to fall, so extra caution is required during this time.
Incorrect removal of ticks: risks and possible consequences
Removing ticks is an important step in reducing the risk of infection with Anaplasma phagocytophilum (anaplasmosis) or other tick-borne pathogens. However, removing ticks incorrectly can lead to an increased risk of infection and other complications. Below are some of the risks and possible consequences of removing ticks incorrectly:
- Transmission of pathogens : If a tick is improperly removed, it may become stressed and release its saliva into the wound, increasing the risk of infection with Anaplasma phagocytophilum (anaplasmoses) or other pathogens.
- Remains of tick parts : If a tick is removed incorrectly, parts of the mouthparts or head can become stuck in the dog's skin. This can lead to inflammation, infection or allergic reactions.
- Squeezing the tick's body : If the tick is crushed during the removal process, its stomach contents can leak into the wound, which also increases the risk of infection.
To minimize these risks, the following steps should be followed to remove ticks correctly and safely:
- Using tick tweezers or tweezers : Use special tick tweezers or fine tweezers to grab the tick as close to the dog's skin as possible. Avoid removing the tick with bare fingers or non-specific tools.
- Slow and Continuous Pulling : Slowly and steadily pull the tick straight out without twisting or squeezing it. Pulling slowly signals the tick to let go, minimizing the risk of saliva transfer or tick parts getting stuck.
- Disinfecting the bite site : After the tick is removed, thoroughly disinfect the bite site and hands with an appropriate disinfectant to reduce the risk of infection.
- Monitoring the Dog : Monitor your dog over the next few days and weeks for possible signs of infection, such as fever, lethargy, or joint pain. If you suspect an infection, seek veterinary advice immediately.
Anaplasmosis FAQs
What is Anaplasmosis?
Anaplasmosis is a parasitic infectious disease caused by Anaplasma species and transmitted by ticks.
How is anaplasmosis transmitted?
Anaplasmosis is transmitted by ticks that carry Anaplasma pathogens. The transmission takes place 24 hours after the start of the sucking act.
What are the symptoms of anaplasmosis?
Symptoms of anaplasmosis can occur in acute and chronic phases. Typical symptoms in the acute phase include fever, apathy, gastrointestinal disorders, splenomegaly, lymphadenopathy, thrombocytopenia, nosebleeds, bleeding gums, petechiae, lameness and polyarthritis. In the chronic phase, pancytopenia, uveitis, lameness, polyarthritis and neurological disorders may occur.
How is anaplasmosis diagnosed?
Diagnosis is carried out by direct pathogen detection using a Giemsa-stained blood smear or PCR from blood in the acute phase or by indirect pathogen detection using antibody detection (titer) using IFAT or ELISA in the chronic phase.
How is anaplasmosis treated?
In the case of acute symptoms with corresponding changes in the blood count, treatment is carried out with an antibiotic. Elimination of the pathogen is often not achieved with Anaplasma platys, but elimination of the pathogen is possible with Anaplasma phagocytophilum. In the chronic phase, monitoring with blood counts, clinical chemistry and protein electrophoresis every 6-12 months is recommended.
How to prevent anaplasmosis?
To protect against anaplasmosis, the use of spot-ons and/or collars containing permethrin and flumethrin is recommended. Behavioral prophylaxis by avoiding tick areas is also useful.
Consequential damage caused by anaplasmosis
Although anaplasmosis in animals is usually easy to treat, in some cases secondary damage can occur, especially if the disease is not recognized and treated in a timely manner. The possible consequential damage depends on the severity of the infection and the organs affected. Some of the possible consequential damages are:
- Joint inflammation and lameness : The inflammatory reactions caused by the bacterium Anaplasma phagocytophilum can lead to joint inflammation and lameness. In some cases, this can lead to permanent joint damage and chronic pain.
- Organ damage : If the anaplasmas cause inflammation within the organs, organ damage can occur. The most commonly affected organs are the liver, kidneys and lungs. Untreated organ damage can lead to impaired organ function and, in the worst case, organ failure.
- Anemia : A reduction in blood platelets (thrombocytes) can lead to bleeding and anemia. In severe cases, this can be life-threatening and require a blood transfusion.
- Neurological symptoms : In rare cases, anaplasmas can also affect the nervous system, which can lead to neurological symptoms such as incoordination, seizures or paralysis.
In order to minimize the risk of consequential damage, it is important to detect and treat anaplasmosis early. If you notice symptoms in your pet that could indicate anaplasmosis, contact a veterinarian immediately. Early and appropriate treatment can help reduce the likelihood of secondary damage and maintain your pet's quality of life.
Summary and conclusions
Anaplasmosis is a tick-borne disease that can cause serious health problems in dogs or cats. Early diagnosis and treatment are crucial for the animal's recovery. To protect your dog or cat from anaplasmosis and other tick-borne diseases, it is important to carry out regular tick prophylaxis and check your animal for ticks. By taking these protective measures, you can help keep your four-legged friend healthy and happy.
Current research on anaplasmosis in dogs
Research into anaplasmosis in dogs/cats is an ongoing process to deepen the understanding of the disease, develop more effective diagnostic and treatment methods, and improve the prevention of tick transmission. Some current research areas are:
- Epidemiology and distribution : Researchers continue to study the occurrence and geographic distribution of Anaplasma phagocytophilum in different regions and in different animal species. These studies help to identify risk areas and times in order to develop targeted prevention measures.
- Resistance to tick agents : Since tick agents play an important role in preventing anaplasmosis, the development of resistance to these agents is also being investigated. The results of these studies may help develop more effective tick treatments or alternative approaches to tick control.
- Improved diagnostic methods : Research aims to develop more precise and faster diagnostic methods for anaplasmosis. This can help detect the disease early and initiate treatment more quickly to minimize possible subsequent damage.
- New therapeutic approaches : The development of new therapeutic approaches, including alternative antibiotics or immunotherapies, may help improve the treatment of anaplasmosis and overcome possible resistance to existing treatments.
- Immunology and pathogenesis : A better understanding of immune responses in anaplasmosis and the mechanisms by which Anaplasma phagocytophilum infects cells and triggers inflammation may help identify new therapeutic targets or prevention strategies.
The results from these areas of research can help reduce the risk of anaplasmosis in dogs/cats, optimize the diagnosis and treatment of the disease, and improve the quality of life of affected dogs.
